Updated January 29, 2024
Insomnia
What this section covers:
-
Am I sleep-deprived?
-
What is normal sleep?
-
Sleep changes with aging
-
Causes of insomnia
-
Diagnosis of insomnia in the clinic
-
Treatment of insomnia
-
Key points

Am I sleep-deprived?
One way to figure out whether insomnia is a problem for you is to determine your degree of sleep deprivation. Check out the “quiz” below to help evaluate this possibility.

If you answered yes to ANY of these questions, insomnia may be a problem.
Insufficient sleep can affect your reaction time, judgment, and other cognitive
functions.
Insufficient sleep can cause you to have difficulty focusing your eyes.
One of the most critical activities that insufficient sleep influences is driving.
Sleep deprivation can make you
dangerous on the road!
What is normal sleep?
On a normal night of sleep, you would fall asleep within about 20 minutes from the time your head hits the pillow. You would sleep about 8 hours, on average. You may get up to urinate at night, but you would easily fall back to sleep. You would awaken feeling rested.

If we were to monitor your sleep overnight in the laboratory, we might see that you cycle through different stages of sleep, alternating between REM (dream) sleep and restful slow-wave sleep, and from light Stage 1 sleep to deep Stage 4 sleep. Stages 3 and 4 sleep are the most restful, but all sleep stages are important.
Individual Sleep Needs Differ
Some individuals are lifelong “short sleepers” who need only 5 or so hours of sleep to be completely rested, while others are “long sleepers” who need 10 or more hours of sleep. Both patterns are normal.
Sleep Changes with Aging
Contrary to a widely held belief, as you get older, you have the same sleep requirements that you did when you were younger. Because of changes in the brain associated with aging, however, you may spend less time in Stages 3 and 4 deep sleep and less time sleeping overall.
About half of people over 65 years have insomnia. This can be trouble falling asleep or trouble staying asleep through the night.
For some, the problem is only intermittent or is time-limited. For those who have this problem every night -- true insomnia -- there may be habits or conditions that are causing or contributing to poor sleep.

To explore this possibility, a personal sleep diary can be used. A sample diary from the American Academy of Sleep Medicine is shown below.

Some seniors find that when they see their sleep and their habits mapped out like this, the problem is obvious; they don’t need to see a doctor. For example, one patient realized that every time his tennis game was moved to 4:00 pm, he had trouble sleeping that night. We’ll talk more about that issue below.
More often, the problem is not so simple, so let’s take a closer look. When you complete your diary, you may find that your sleeplessness often occurs at a particular time of night, as shown on the chart below. The green blocks with the “z” represent sleep.
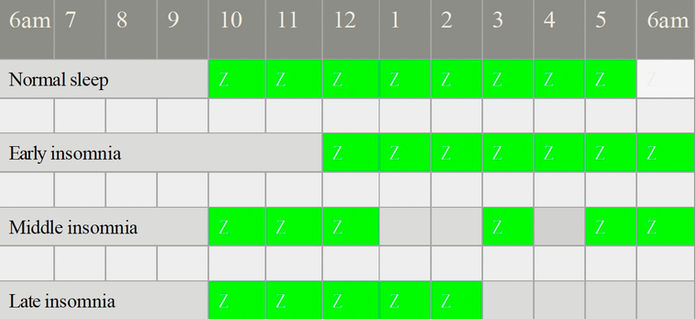
Early insomnia means you have trouble falling asleep. Two things that are commonly associated with early insomnia are stress and anxiety, but there are other causes.
Middle insomnia means your sleep is disrupted during the night. This pattern can be associated with pain that awakens you, breathing problems such as sleep apnea, and conditions like Parkinson’s disease.
Late insomnia is also called early morning awakening. This pattern is characteristic of depression as well as drug effects — caffeine, nicotine, or alcohol — discussed further below.
Causes of Insomnia

Medical Conditions
-
Pain
-
Restless legs
-
Breathing problems
-
Heart problems
-
Thyroid disease
-
Parkinson’s disease
Pain from arthritis or neuropathy is a common cause of insomnia in elders, often associated with middle insomnia. Restless legs can disturb sleep patterns without even waking you up, so you’re not aware of the disturbance. An overnight sleep study (see below) can help diagnose this condition.
Breathing problems that interfere with sleep include sleep apnea, asthma, and chronic obstructive pulmonary disease (COPD). Heart problems that disrupt sleep include angina, arrhythmias, and congestive heart failure (CHF). Thyroid disease – particularly overactive thyroid or hyperthyroidism — also can be associated with insomnia.
Many individuals with Parkinson’s disease report poor sleep, and this is due to several factors, including reduced levels of dopamine, which helps to regulate sleep-wake cycles, inability to shift position in bed because of stiffness, and the high prevalence of sleep apnea in this population.
Medications that may cause Insomnia
It makes sense that any drug you use to help you wake up in the morning may cause insomnia at night. Likewise, many medications have stimulant effects. These include the following:
-
Stimulants: theophylline, Ritalin, amphetamines
-
Over-the-counter pain pills that contain caffeine: Excedrin, Anacin
-
Decongestant cold medications
-
Antiarrhythmics, beta blockers, statins
-
Steroids
-
SSRI antidepressants (Lexapro, Celexa, Prozac, etc.)
-
Parkinson’s disease drugs: Sinemet
-
Thyroid replacement medication (at high doses)
-
Memory-enhancing drugs such as donepezil, galantamine, and rivastigmine (because of increased dreaming)
-
Herbal supplements: St. John’s wort, Sam-e, and ginseng
Psychological causes of Insomnia
Everyone has experienced the effects of stress and worrying on sleep. These effects may be short-lived if the stress resolves. Untreated depression and anxiety disorders, on the other hand, may cause persistent insomnia.

Habits as a cause of Insomnia
-
Caffeine
-
Smoking
-
Alcohol
-
Sedentary lifestyle

Caffeine
Caffeine is well known to cause problems with sleep, and caffeine is present not only in coffee and tea, but also energy drinks, many soft drinks, and chocolate. The Center for Science in the Public Interest has published a long list of specific, branded beverages and foods with their caffeine content, which is available on the web.
Many people find that their tolerance for caffeine drops as they get older so that sleep starts to be affected. That is, unless they cut down and limit intake to the morning hours, they’ll have trouble.
Those who insist that caffeine isn’t the problem — “I drink coffee after dinner every night, and I fall asleep fine; it’s waking up at 4:00 am that’s the problem” -- should consider the graph below.

The graph shows that the levels of natural chemicals such as melatonin present at high concentrations at the usual bedtime decline over the sleep period, while levels of wake-promoting chemicals such as orexin increase over the sleep period. At some point during the night, when the tide is turning in favor of wakefulness, caffeine (which is still in the system) can accelerate the waking process, causing early morning awakening.
Smoking
Nicotine is another culprit. Because nicotine is a stimulant, and because it is cleared from the body more slowly with aging, it can significantly affect sleep in seniors. Those who smoke have less deep sleep and less dream sleep, and awaken more easily from light sleep. In addition, elderly smokers might find that they wake up during the night in nicotine withdrawal, fueling the need to smoke immediately.


Alcohol
Drinking alcohol has definite sleep effects. Although having “a few stiff drinks” can help you fall asleep, it won’t help you stay asleep; just the opposite. When your body begins to withdraw from alcohol during the night, you wake up. In addition, like smokers, drinkers have less deep sleep and less dream sleep. Drinkers also have an increased risk of falls when they get out of bed to urinate.
Sedentary Lifestyle
Lack of exercise is another factor. A sedentary lifestyle contributes to insomnia by depriving your body of clear-cut day/night signals.
Conversely, getting exercise helps promote sound sleep if it is not too close to bedtime.

Poor Sleep Hygiene as a cause of Insomnia
What is "sleep hygiene"?
Hygiene is defined as the conditions or practices that are conducive to maintaining health and preventing disease. In the context of sleep, it refers to personal habits that promote sound sleep.
Personal habits that contribute to insomnia include the following:
-
Varying bedtimes from night to night
-
Excessive daytime napping
-
Lying awake in bed (for hours)
-
Maintaining a poor sleep environment
-
Watching TV or using a computer or phone in bed
To recap: so far, we’ve discussed five factors that affect sleep:
-
Medical conditions
-
Medications
-
Psychological issues
-
Habits: caffeine, smoking, drinking alcohol, sedentary lifestyle
-
Poor sleep hygiene
Diagnosis of Insomnia in the Clinic and Laboratory

If you were to come to the clinic for an evaluation of sleep problems, a great deal of attention would be paid to these habits or conditions and how they could be eliminated.
Further information about the exact nature of the sleep disruption could be obtained through an overnight sleep study known as a polysomnogram (PSG).
The PSG records brain waves, breathing patterns, blood oxygen level, pulse, eye movements, and limb movements. Ideally, the test is done in the laboratory, but a take-home monitoring system is also possible.
PSG is most often used to confirm a diagnosis of sleep apnea, but it yields other information helpful to the clinician, and can confirm the pattern of sleep disruption.
Treatment of Insomnia
Any plan to treat insomnia would first require the treatment of medical conditions such as pain and sleep apnea. Medications would be reviewed in detail, and any offending drugs discontinued or substituted. Strong recommendations would be made to cut down or cut out smoking and drinking alcohol. Exercise would be recommended during the morning or early afternoon hours. Some seniors have found that exercising 6-8 hours before bedtime has the most beneficial effect on nighttime sleep.


Next, attention would be focused on optimizing the sleep environment. It should be dark and as quiet as possible. It should be maintained at the right temperature for you — not too hot and not too cold. Some thought should be given to what is the correct mattress, pillow, and bedding for you.
Good sleep hygiene would be reinforced. This means keeping a regular schedule for going to bed, avoiding excessive napping during the day, and using time in bed only for sleep and sex. It is recommended that you avoid spending nighttime hours lying awake in bed. If you find that you cannot sleep despite measures taken, you should get out of bed and read a book, take a hot bath, or listen to soothing music.
Outdoor activities such as swimming would be recommended. Exposure to bright light in the morning is activating, can help to reset the circadian “clock,” and promotes nighttime sleep.

Relaxation at bedtime can be promoted with a warm bath or shower, soothing music, chamomile or Sleepy Time tea, or a bedtime snack of tryptophan-containing foods along with complex carbohydrates (e.g., avocado, turkey, and strawberries with whole grain bread or potato salad).

Finally, before we get to the topic of sleep medication,
there is one more trick that can be tried if you find that you have problems falling asleep and are waking up later than you wish. This is called sleep restriction.
This technique involves the following steps:
-
Set an alarm for the time you wish to wake up.
-
Stay awake all day (no naps).
-
When the alarm rings, get up and start your day.
-
As you continue this practice, your brain’s sleep clock should reset after a few nights.

Sleep Medications
There’s a reason that sleep medications are considered last among treatment options, and that is that drugs are in fact the last resort. All medications have side effects, and some of the sleep medications are the worst offenders. Older drugs once used for insomnia, such as chloral hydrate, methaqualone, and Valium, are not recommended because of dangerous side effects, tolerance, and addiction potential.
What might surprise you is that over-the-counter sleep aids have side effects that are often worse than commonly used prescription drugs. For older individuals, drugs such as Benadryl, Nytol, Sominex, Tylenol PM, and Unisom are not recommended because of side effects such as constipation, urinary retention, blurred vision, and memory impairment. These are called “anticholinergic” side effects.
Quite a few prescription medications are now available to treat insomnia. Several of the most tried-and-true are drugs used for other indications that were repurposed for insomnia. These include trazodone, mirtazapine, doxepin, and gabapentin.

Trazodone
This drug is inexpensive and generally has few side effects and few drug interactions, although it may cause a blood pressure drop on standing in some patients. A typical dose is 25-50 mg at bedtime.
Mirtazapine
This is an antidepressant that is highly sedating at a very low dose of 3.75 to.7.5 mg at bedtime.
Mirtazapine also promotes appetite, so weight gain should be expected.


Doxepin
This drug is an older tricyclic antidepressant that is useful at very low doses to treat insomnia. It has been studied in older adults and found to be safe in treating early and middle insomnia.
Doxepin is started at a dose of 3 mg. If this dose is ineffective, the dose is increased to 6 mg. Doses above 6 mg should not be used in seniors because of anticholinergic side effects mentioned above.
Gabapentin
This drug is used for painful neuropathy and seizures, and treats insomnia at a low dose of 100 to 300 mg. In recent years, recognition of the addiction and diversion potential of this drug has greatly limited its use for this indication.


Ramelteon
This drug works for early insomnia (trouble falling asleep), but not to maintain sleep through the night. It does have drug interactions, and can be associated with next-day hangover. In addition, it is associated with nighttime behaviors such as sleepwalking and sleep driving.
Melatonin
This is a naturally occurring hormone in the body that is available over the counter in synthetic form to treat insomnia. (A non-synthetic form made from the pineal glands of animals is not recommended because of potential viral contamination.)
Melatonin is generally safe, although not recommended for those with dementia. Melatonin does interact with numerous other medications, including blood thinners and drugs for hypertension and diabetes. Common side effects are drowsiness, dizziness, headache, and nausea. Confusion may be seen.
Widely varying dosages are recommended in the literature, but personal prescribing experience suggests that a dosage of 1 to 5 mg 2 hrs before bedtime works for many patients.

Benzodiazepines
This class of drugs that includes Valium, Ativan (lorazepam), and Restoril (temazepam). Although these drugs are sedating, they are not recommended for use in elders because of side effects that include daytime sleepiness, unsteady walking, slowed reaction time, and memory problems. These drugs are infamous for addiction and diversion potential and for tolerance to sleep-inducing effects over time.
Benzodiazepine derivatives
These are the “Z” drugs: zolpidem (Ambien), zaleplon (Sonata), and eszopiclone (Lunesta), which were intended to be safer alternatives to the benzodiazepines. Among seniors, however, these drugs have not proven to be safe because of an increased risk of memory impairment, daytime drowsiness, falls with fracture, and motor vehicle accidents. These drugs are not recommended for individuals over 65 years.
Seroquel (quetiapine)
This drug is an antipsychotic formerly used to treat insomnia at a dose of 25 mg at bedtime. This drug is not recommended as a treatment for insomnia because of serious side effects that include death in seniors with dementia.
The newest sleep medications: orexin receptor blockers
These drugs block the action of the wakefulness-promoting hormone orexin to maintain sleep.

Suvorexant (Belsomra) FDA approved 2014
This drug has been promoted to treat early and middle insomnia, and touted to be safe and effective in elders, but some users have found it ineffective, and others have reported adverse effects such as hangover effect, nightmares, sleepwalking, and agitation.
The dose is 10 mg taken 30 minutes before bedtime with at least 7 hours left of sleep time before planned awakening.
Drug interactions with antibiotics, antifungals, and many other drugs necessitate a lower dose of 5 mg when these other drugs are taken.
Lemborexant (Dayvigo) FDA approved 2019
This drug was approved in 2019 to treat insomnia. It is reported to be be effective and safe at 5 mg taken just before bedtime with at least 7 hours left of sleep time. Caution is advised for elderly patients because of somnolence and drowsiness associated with falls. Higher doses introduce a greater risk of next-day somnolence.


Daridorexant (Quviviq) FDA approved 2022
This drug should be taken within 30 minutes of bedtime, with at least 7 hours remaining before planned awakening. The drug is available in 25 mg and 50 mg doses, with the 50 mg dose being optimal for elderly patients as well as younger adults. The drug does not need titration from 25 to 50 mg, but the lower 25 mg dose may be required for patients taking medications such as diltiazem, and the drug is contraindicated for patients taking strong CYP3A4 inhibitors.
Key points
-
Normal sleep — fall asleep in about 20 minutes, sleep about 8 hours, awaken refreshed.
-
Deep sleep (stages 3 & 4) is most refreshing.
-
Sleep changes with normal aging — less time in deep sleep, reduced hours of sleep. These changes are a problem for only about half of elders.
-
Many factors may interfere with sleep — medical problems, medications, psychological issues, habits like smoking or drinking, and poor sleep hygiene.
-
Treatment involves addressing these factors. The most important one is improving sleep hygiene.
-
Sleep medications can appropriately be used to treat seniors, but only as a last resort, after all other factors have been addressed.